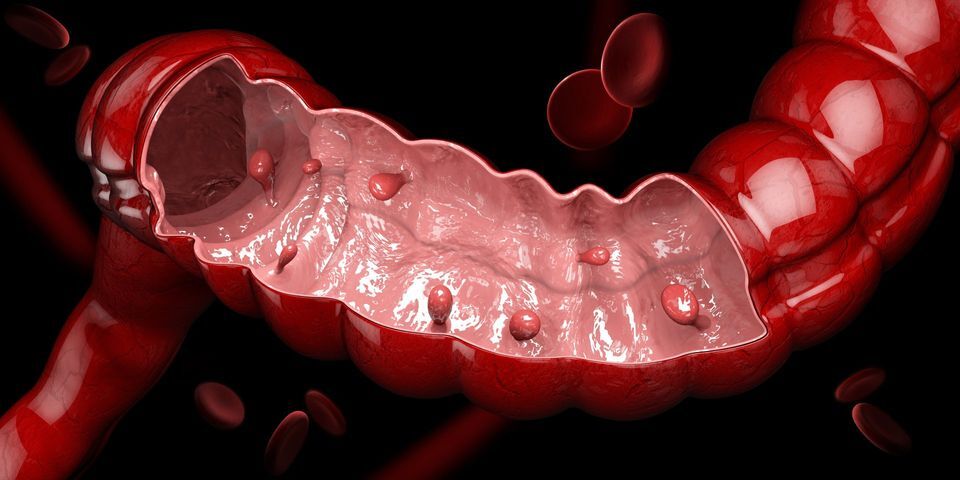
Colonic polyps are a precursor of colon cancer, the second deadliest type of cancer in the United States. These polyps, also known as colorectal polyps, are small growths that can be found on the colon’s surface and the rectum. Polyps form when cell division occurs at higher than normal rate. However, not all colorectal polyps develop into colorectal cancer, but due to the high likelihood that they will, they need to be removed by a gastroenterologist.
Symptoms of Colorectal Polyps
While many patients don’t have any symptoms, some signs can trigger red flags when it comes to colon polyps. Chronic polyps can be identified by:
- Blood in stool
- Constipation
- Diarrhea
- Pain using the bathroom
- Vomiting
- Nausea
Causes of Colorectal Polyps
While colorectal polyps impact a patient that has no risk factors, there are a variety of conditions and scenarios that lead to the development of colon polyps. The screening guidelines for colorectal cancer have recently been lowered to 45 years from 50 years. However, with a family history, you may need to be seen sooner. Other factors that lead to colorectal polyps include:
- Type II Diabetes
- Smoking
- Obesity
- IBD
- Crohn’s Disease
Treatment for Colorectal Polyps
Treating, managing, and resolving some of the causes listed above can abate colorectal polyps. However, once developed, immediate removal is the most effective treatment for colon polyps. This can be performed during a routine colonoscopy.